
What is ERCP?
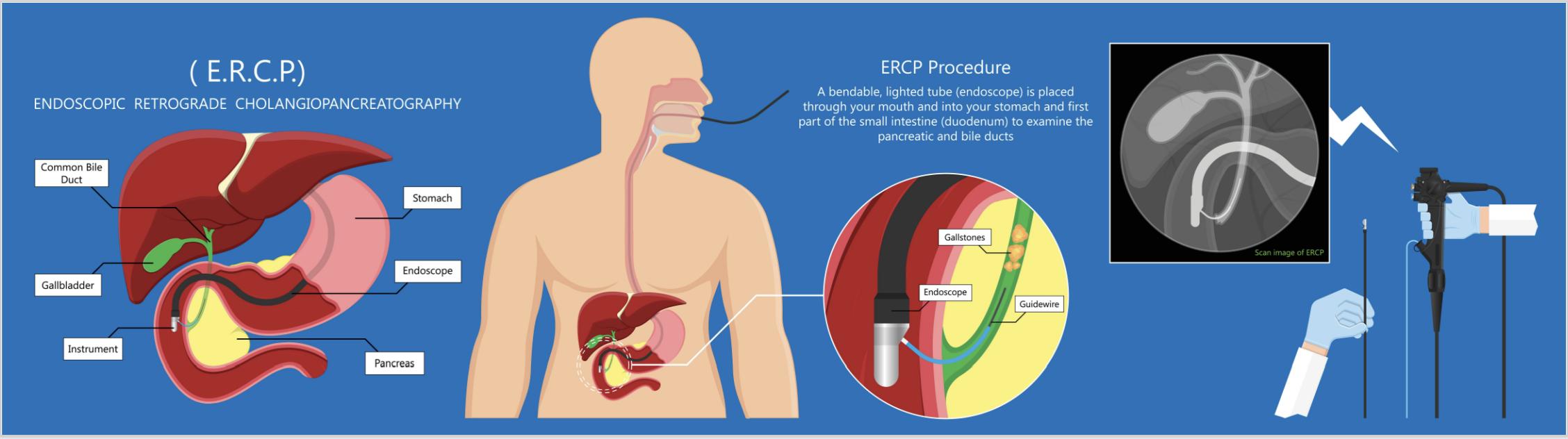
Endoscopic retrograde cholangio-pancreatography (ERCP) is a type of endoscopic procedure that may be used to treat problems in the bile and pancreatic ducts. It uses an endoscope (a thin, flexible tube with a camera and light) combined with x-ray images to examine the bile ducts, pancreatic ducts, and gallbladder.
ERCP is a highly specialised procedure which requires advanced training. Rest assured that Dr Keegan has undertaken extensive training in this procedure in centres of excellence in Australia, the United Kingdom, and France, and his training and credentials have been recognised in Australia by the Conjoint Committee for Recognition of Training in Gastrointestinal Endoscopy.
Why is ERCP performed?
After diagnosis (often by CT, MRI, or endoscopic ultrasound), ERCP is performed to treat problems in the bile ducts, pancreatic ducts, or gallbladder. It can be used to remove gallstones, treat blockages, and take tissue samples for further testing. It may be uses to treat complications after surgery. The procedure is generally the least invasive way to treat these issues (compared with through-the-skin radiologic procedures or surgery).
What can I expect?
During ERCP, you will be given medication to help you relax and feel comfortable. For many patients this is sedation similar to when having a colonoscopy, though in some situations, an anaesthetist may advise you to have a general anaesthetic. The endoscope will be inserted through your mouth and down your throat. You may feel some pressure or discomfort during the procedure or for a short time after the procedure, but it should not be painful. If a stent is placed, this can be uncomfortable in the first 24-48 hours. More significant symptoms should be discussed with your gastroenterologist and nursing staff.
How do I prepare?
Before the procedure, you will need to fast for 6 hours. Water only (or black tea/coffee without milk or other additives) can be consumed in small quantities until 2 hours prior to your procedure. You may also need to stop taking certain medications, and your current medications need to be provided to your gastroenterologist in advance of your procedure. Your doctor will give you personalised instructions on how to prepare for the procedure. Measures to reduce the risk of pancreatitis with your procedure may be advised, and can include intravenous hydration and/or an anti-inflammatory suppository (rectal medication) prior to your procedure.
Do I need to stay in hospital?
In most circumstances, ERCP is performed as an outpatient procedure, though some patients may already be hospitalised for other reasons. If you have new symptoms after the procedure you may be asked to stay in hospital for observation or investigation, so it is advisable to have some belongings with you, or packed with a friend or relative who can bring them to you if this is the case.
What are the risks?
Like any medical procedure, there are risks associated with ERCP, though these are rarely encountered. These include bleeding, infection, pancreatitis (inflammation of the pancreas), perforation (a hole in the intestine or ducts), and reaction to anaesthesia, along with other rarer issues. In conventional ERCP, pancreatitis can affect 3-7% of patients. For most patients, it is short-lived and without other issues, though in rare circumstances can be more significant. The risks can be reduced with pre-procedure measures and endoscopic techniques. Patients with conditions where the risks are suspected to be higher will have this discussed ahead of any procedure. For most patients, risks of procedural complication are seen to be much less likely than the risk of not addressing the issue for which you have been referred. When this is not clearly the case, further assessment and discussion will be required.
What do I do after my procedure?
After the procedure, you will need to be observed for a short period of time before you can go home. You may experience some mild discomfort or bloating for a few hours after the procedure. Rarely, if there are more significant symptoms you may be asked to stay overnight for observation or investigations. Your doctor will give you specific instructions on what to do after the procedure, especially if there have been biopsies or your procedure was performed to treat an infection or other significant active medical issues. If significant new symptoms arise in the first 24 hours after your procedure, these should be raised immediately, either with your gastroenterologist or the hospital ED if out of hours.
